When you hear about billion-dollar health scams, you immediately think it’s a huge corporation that is bilking the little guy out of something. Yet there’s another health scam that’s been going on for years, and the government doesn’t want to stop it. Let’s look at what this health scam is.
Using Health Insurance Wisely
When you’re at a government job, you get government-funded health insurance for your immediate family. But what happens when you sign someone up who’s not your family?

The big health scam that’s been the racket over the last few decades is signing up people for health insurance that isn’t supposed to be covered based on the limits of the coverage.
A Few Examples Stand Out
One man signed up for his sister and niece in his federal health benefits plan. He made them pose as his wife and stepchild to ensure they were technically covered.

Another man covered his ex-wife under the federal plan for years. His fraud only came to light when he remarried and tried to add the new wife to the plan.
A Three-Billion-Dollar-a-Year Problem
Federal officials have calculated the amount of money the government spends on fraudulent coverage, averaging out to around $3 billion a year in taxpayer money.

Yet it’s one of the simplest things a federal employee can do. It’s so hard to get caught that there’s no solid record of how many people are committing this fraud, but there may be a lot.
A Tedious Job To Manage
The responsibility of managing health insurance for federal employees falls to the Office of Personnel Management (OPM). The OPM dishes out around $60 billion per year in insurance costs.

However, according to the Government Accountability Office (GAO), the OPM hasn’t verified the validity of the people it covers. It assumes that federal employees know the rules and works from there.
A Bill Pending Oversight
Republican Rick Scott (R-Fla.) thinks this is unacceptable. He intends to introduce a bill in March that forces the OPM to audit its members. He claims it’s costing taxpayers billions of dollars.

He’s also noted that the OPM arguably doesn’t care about fraud, or they would have already performed an audit. He outlines that both companies and states do audits often enough.
OPM Lashes Back
A spokesperson for the OPM took offense at the insinuation that the office doesn’t care about fraud. They went on to state that the OPM is taking the necessary measures to ensure fraud doesn’t propagate.

The OPM gets its funds from Congress, and they are working with state agencies and federal bureaus to ensure that fraud remains at a minimum for the federal health insurance program.
Too Expensive to Audit
Despite the push by the Government Accountability Office and Sen. Scott’s concern, the OPM has stated that it has no intention of undertaking an audit. The amount of resources, both financial and human, would be far too much, the office said.

The office sits at the nexus of over one hundred and sixty government offices and more than seventy health insurance providers, trying to link demand with supply and foot the bill for the insurance plans.
Hitting The Budget Where It Hurts
The OPM already provides health insurance to many federal employees, but an audit would have to come out of that funding, leaving some federal employees potentially without coverage.

Federal employees’ health comes first to the OPM, and to this end, they are not interested in spending any portion of their funding on what they see as a useless audit.
No Easy Fix For This Problem
It may seem that an audit could fix this entire mess, but the truth is that the problem is multi-faceted. While it is a costly problem to address, avoiding it could be more costly.

With as much as $3 billion of the OPM’s budget claimed by people whom it shouldn’t be covering, it’s already a significant burden on the office’s resources.
Seemingly Unconcerned
The GAO says that while the OPM says it’s interested in fixing the problem, its actions say something else. Seto Bagdoyan, who authored a report on the problem in 2022, says Congressional oversight may be the only way to address the issue.

Scott’s bill wouldn’t offer the OPM any new funding to undertake an audit. However, it would force the office to implement several measures suggested by Bagdoyan’s report.
Could See Bipartisan Support
Scott believes his bill will see bipartisan support because it’s an issue that affects all Americans, not just one party or the other. He noted that it would benefit everyone.

Jokingly, the senator said that unless a candidate was elected on a platform that supported fraud in public office, he didn’t see how someone would vote against the measure since it helped the government keep a clean house.
Not New to Auditing Government Health Plans
Overspending and auditing government health plans is not a new portfolio for Scott. When he became governor of Florida, he audited the state health plan and found that 3% of the people it covered were ineligible, saving the state $20 million.

Audits in California saved the state $122 million from 2.6% of enrollees that were ineligible for coverage. Yet, the OPM still has no plans to conduct an audit. That doesn’t mean they’re not doing anything about it.
Using A Master Enrollment Index
What’s the OPM’s strategy to clean up the enrollment records for federal coverage? They intend to use the new FEHB Master Enrollment Index, a list of federal employees and their family members.
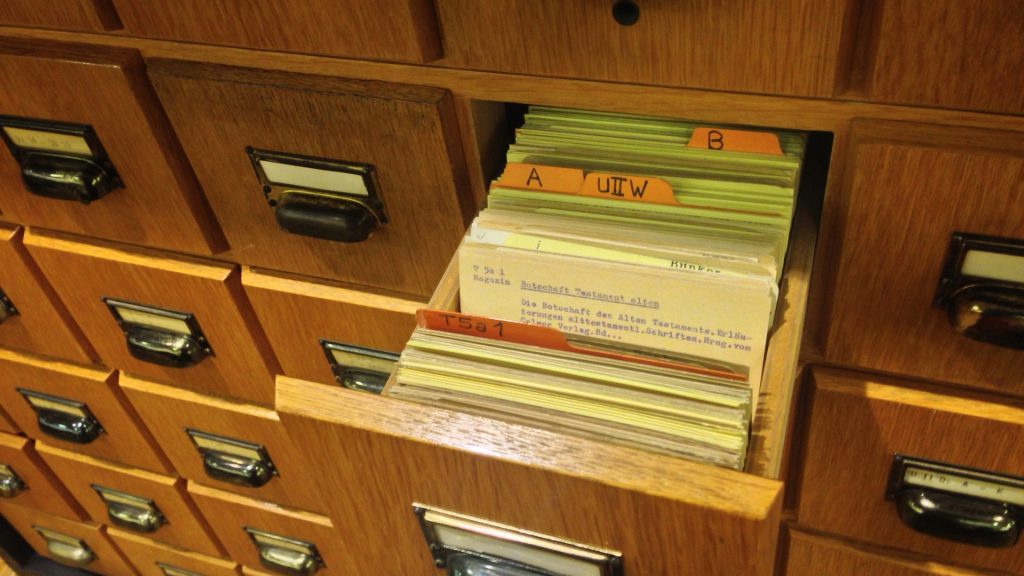
The idea is that cross-checking this list against those who are enrolled in the system will help them determine who is and isn’t eligible for the program. The OPM also uses an independent system alongside the enrollment index to ensure it gets it right.
Setting An Example
The OPM is responsible for setting an example as the manager of the largest self-funded insurance provider in the country. They are dealing with taxpayer money, so they should try to save the taxpayer as much as possible.

Unlike what most people think, federal insurance coverage is not “free money.” It’s all of our taxes going into paying for federal employees’ healthcare. Abusing this system hurts everyone, most especially the taxpayers.